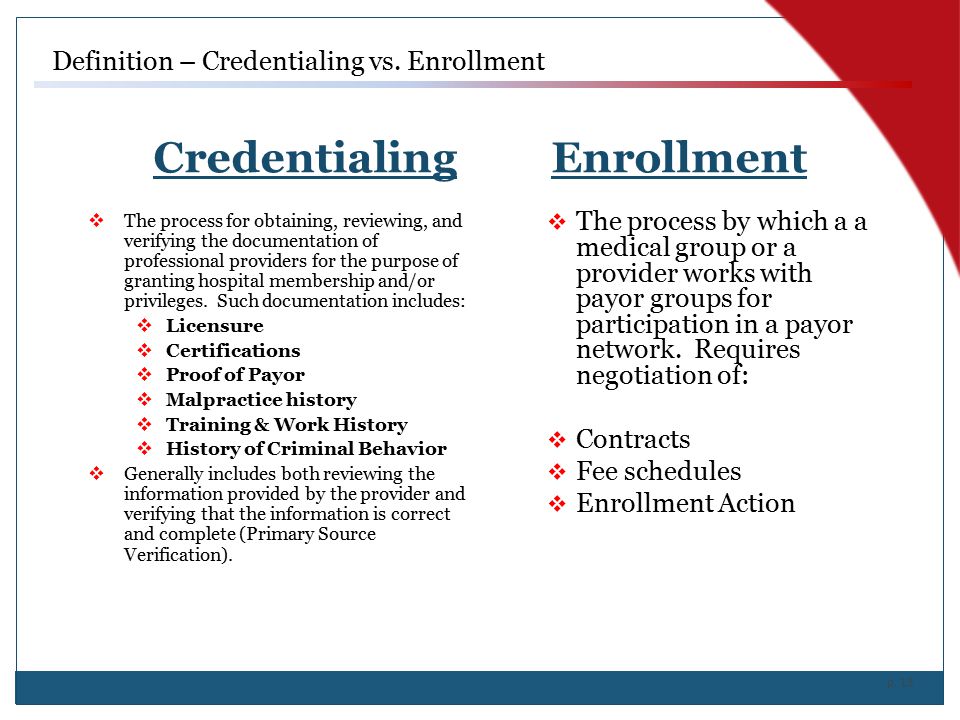
The insurance credentialing process is required for providers to be considered "participating" with an insurance company. The goal of the insurance credentialing process is to become in-network, which prevents your patients from incurring high out of pocket costs associated with seeing an out-of-network provider. In turn, you have the opportunity for an increase in insured patients as well as paid claims.
Let us help you with:
- CAQH Registration & Enrollment as well as Quarterly Attestation management
- NPI registration (Type I and Type II)
- Individual & Group Medicare Enrollment
- Medicaid Enrollment for Group & Individual
- Telemedicine Credentialing
- Commercial insurance provider enrollment and credentialing (i.e., Aetna, BCBS, CIGNA, HAP, TriCare, Humana, United Healthcare and many more!)